Chapter 6 - Strikes and Bites
6. Strikes and Bites
When
a snake bites a man the effects are extremely variable and unpredictable. They
range from transient and local discomfort…to collapse and death within a few
minutes.
Sherman and Madge Minton, 1980
Fascination
with rattlesnakes led me to keep as many species as I could collect or buy in
the late 1960’s. The first Mojave Rattlesnake (Crotalus scutulatus) I kept in
captivity taught me that venom can act astonishingly fast and that scutulatus
is exceptionally dangerous. Observations made during feeding many species
rattlesnakes did not prepare me for the rapid and deadly nature of Mojave
Rattlesnake venom. Within 15 seconds of introducing a white mouse to the cage
housing the 80 cm scutulatus, the snake struck the mouse and released it. The
mouse instantly started to bleed from its eyes, mouth, ears, anus, tail, and
died. The combination of highly toxic venom and an efficient venom delivery
system makes scutulatus one of the most dangerous snakes in North America.
Hands-on-learning is not always safe, but it tends to create vivid memories not
easily forgotten.
The unpredictable nature of venomous snakebite
referred to by the Mintons is poorly understood by the general public. Many
physicians are unfamiliar with the stochastic nature of envenomation unless
they work in an area with venomous snakes. The unpredictability is at the heart
of much of the snakebite mystique. Yet it has been long known to
herpetologists; the literature is full of stories of people suffering no
symptoms from a venomous snakebite while others experience a quick death. Oddly,
others bitten by harmless snakes may show signs of envenomation. Consider the
following stories from India.
A
boy cutting grass close to a bungalow was bitten on the foot by a krait. He
continued to work, but eventually stopped because of increasing pain. When his
family discovered the situation, they held a candle in front of him and asked
him how many flames he saw; he replied five. This was considered a symptom of
poisoning so the boy was brought to a local medicine man, or Mantri, who used
incantations. Unconscious before he arrived, his teeth were firmly clenched and
oral medicine could not be administered. The family believed the case hopeless,
however, the Mantri soon brought the boy back to a conscious state and he
recovered completely.
In
a second instance an 18-year-old male was bitten while lying down. He began
vomiting and went into a stupefied state of consciousness. A Mantri had given
the patient powdered root while repeating an incantation. An observer retrieved
the dead snake and found it to be a young Dhaman, a large, harmless, colubrid
snake. The boy was assured he was in no danger, but he fainted again and his feet
and hands became very cold. Eventually, the boy recovered.
What
explains these stories? In the first case, it seems likely that if the snake
was actually a krait (Bungarus) and not a similarly colored and patterned wolf
snake (Lycodon), or other harmless species, little or no venom was injected
during the bite. This is not uncommon. The literature suggests that 30–50% of
defensive bites by venomous snakes are dry bites. In a dry bite no venom is
injected. If venom is injected, there is a good chance it will be a sub-lethal
dose. However, kraits are nocturnal and the boy was most certainly cutting
grass during the day. Krait venom does not produce pain at the site of the
bite, but cobra venom would. Using a candle may reveal double vision (diplopia),
a common symptom of neurotoxic envenomation, and the clenched jaw demonstrates
flaccid paralysis had not occurred. The presence of some symptoms and the
absence of others suggest the boy was suffering from self-induced fear.
The
second instance is likely due to the power of suggestion. If the human brain is
expecting something to happen, it may, in fact make the expected results appear
within the body. This phenomenon is well known and commonly demonstrated in
hypnotism, and the placebo effectseen in medical trials. Both are based upon
the power of suggestion. The human mind is easily deceived because the
imagination is a powerful tool and mind and body are not separate entities.
Dwelling on the consequences of snakebite may induce anxiety, hyperventilation,
faintness, a slowed heartbeat, and a variety of other symptoms that mislead
physicians trying to diagnosis the situation.
At a hospital in southeastern Brazil, over
the course of 34 consecutive months, 40 cases of snakebite with confirmed species
identification involved either a tropical rattlesnake (Crotalus sp.) or a lancehead
(Bothrops sp.). Of 33 bites from the lanceheads, 10 (33.3%) showed no signs of
envenomation. Of the seven rattlesnake bites, three (42.9%) showed no signs of
envenomation. A similar situation was reported by herpetologist Van Wallach who
was bitten on the hand by a Variable Mole Viper (Atractaspis irregularis). He
described swelling, which lasted about three days, extensive pain in muscles,
nerves and lymph nodes from head to toe, and discoloration at the bite site. Even
more interestingly, Wallach wrote that he had been bitten six times by venomous
snakes and in two of these bites (33%) there were no symptoms of venom being
injected. Venomous snakes do bite without injecting any venom. However, lethal
doses of venom are sometimes delivered and death may be rapid or be delayed.
Consider
the case of Joe Slowinski, a 38-year-old herpetologist at the California
Academy of Sciences studying the snakes of Myanmar. While working at a remote field
site on the morning of September 11, 2001 his field assistant brought him a
snake in a bag. The assistant believed it to be a harmless white-banded wolf
snake in the genus Lycodon. Tired,
Slowinski reached into the bag to remove the snake and was bit at the base of
his middle finger. The snake was a Multi-banded Krait (Bungarus multicinctus),
a fact Slowinski immediately noted upon being bitten. Wolf snakes often mimic
kraits very closely in color and pattern, and the assumption that the snake in
the bag was indeed a wolf snake proved fatal. Slowinski died 30 hours later
despite the best efforts of his colleagues to keep him alive using rescue
breathing. Ironically, Slowinski had written a popular article for the
California Academy’s magazine ending it with the following sentence, “The best
way to avoid being bitten by a venomous snake is simply to leave it alone.”
Avoiding
venomous snakes is an excellent way to stay healthy, but avoidance is difficult
if you make a living collecting venomous snakes. It was not practical for
Slowinski, nor was it practical for William Oliver. In 18th century England
venomous snakes were in great demand for their medicinal value, and a few
people made a living collecting and selling snakes to apothecaries. William
Oliver was a viper collector in southwest England, near Bath. On June 1, 1735
Oliver was bitten at the base of his right thumb and, even before the snake had
released its bite, a burning pain shot up his right arm. Oliver’s eyes became
bloodshot and watery. Within the hour he had chest pain, faintness, shortness
of breath, and cold sweats. He was soon vomiting, the arm had swolled
significantly, and he suffered temporary blindness. Oliver, however, had a
remedy ― olive oil, a snakebite remedy he had saved for just such an occasion.
About 75 minutes after being bitten, a dish of glowing charcoal was brought to
him. He held his naked arm over the glowing embers while his wife rubbed the
limb with the oil. The arm was rotated over the coals as if it was being
roasted. It was Oliver’s opinion that the pain from the venom had ceased, but
the swelling remained. His pulse was weak, but he started to drink the olive
oil. He was put in bed and his arm was again treated with heat and bathed in
salad oil. Oliver fell into a sound, nine-hour asleep, and when he awoke in the
morning he was feeling healthy. But, the symptoms returned in the afternoon
after he became intoxicated from drinking rum and beer. The heat treatment was
used a third time and then his arm was wrapped in paper soaked in olive oil. Presumably,
Oliver survived the bite. However, the account reported by his doctor makes no
mention of the long-term effects of the venom or the heat treatment on his arm.
Oliver was bitten by the European Adder
(Vipera berus), a small viper and the only native venomous snake known to
inhabit the United Kingdom. Even in the 21st century, about 100 people sustain
Adder bites each year. Roughly 70% of the victims have no symptoms, or suffer
only from local pain and swelling at the bite site. The other 30% may have more
severe symptoms including nausea, vomiting, diarrhea, sweating, fever,
tachycardia, loss of consciousness, swelling of the face, severe lowering of
blood pressure, bleeding, kidney failure, coma, and seizures. Deaths from Adder
bites are rare but 14 deaths have been documented since 1875, the most recent
was a 5-year old child in 1975
Gourmet
chef Le Hung Cuong, 22, died en route to a hospital in Haiphong, Vietnam on the
20th of August 2002. He was preparing a specialty dish, snake blood soup, when
he lifted a half-meter long sea snake out of an aquarium. The snake thrashed
around and bit his left arm. The restaurant owner believed that Cuong did not
follow the rule of wearing gloves when handling the snake. After the bite, Cuong
dropped the snake back into the tank where another chef picked it up and served
it to a customer. Cuong’s death was quick and probably resulted from respiratory
paralysis.
Envenomation Strategies
In
the mid 19th century, Philadelphia physician, novelist, and venom researcher,
Silas Weir Mitchell described the strike of a rattlesnake and some of the
events that can influence the success or failure of envenomation.
He does not pursue, he waits…Then his head
and neck are thrown far back, his mouth is opened very wide, the fang held
firmly erect, and with an abrupt swiftness, for which his ordinary motions
prepare one but little, he strikes once and is back on guard again, vigilant
and brave. The blow is a stab, and is given by throwing the head forward while
the half-coils below it are straightened out to lengthen the neck and give
power to the motions which drive the fangs into the opponent’s flesh; as they
enter, the temporal muscle closes the lower jaw on and forces the sharp fangs
deeper in. It is a thrust aided by a bite. At this moment the poison duct is
opened by the relaxation of the muscle which surrounds it, and the same muscle
which shuts the jaw squeezes the gland, and drives its venom through the duct
and hollow fang into the bitten part.
In
so complicated a series of acts there is often failure. The tooth strikes on
tough skin and doubles back or fails to enter, or the serpent misjudges distance
and falls short and may squirt the venom four or five feet in the air doing no
harm.
Different
clades of snakes show different strategies in hunting, striking, and
envenomation. The fixed front-fanged elapids tend to have slender bodies and
narrow heads. They actively forage for food, seeking prey in burrows, crevices,
or in the open. Once the prey is located, the typical elapid will seize and hold
the prey with its mouth. Some species also use coils of the body to prevent the
prey from escaping. There are exceptions. The death adders of Australia have
wide heads, thick heavy bodies and wait in ambush for prey, and are convergent
with vipers in many aspects of their morphology and behavior. Taipans also
differ from most elapids because they actively forage for mammals, strike from
a longer distance, sometimes repeatedly, and then release. This behavior may then
require trailing the prey until it is dead.
Vipers
have a different strategy. Like the death adders, vipers are ambush predators
and don’t normally forage for prey by active searching. Instead, they sit and
wait along trails used by prey. These may be a grass-lined runway used by
rodents, the base of fallen logs where small animals will encounter the barrier
and move along the edge, or on a branch of a tree full of fruit waiting for
birds or mammals to approach. After the strike and bite, vipers frequently
release the prey and then trail the bitten prey until it is immobilized by the
venom. As always, there are exceptions. The Cottonmouth (Agkistrodon piscivorus)
will actively forage for food by searching shorelines, though it too, will sometimes
hunt from ambush. Additionally, some of the arboreal species will hold on to
the prey when it is bitten so it won’t be lost.
In
an experiment using 20 Palestinian Vipers (Vipera palaestinae), Elazar Kochva
investigated the volume of venom injected during a bite. Kochva allowed snakes
to bite dead mice that were pre-weighed. Then, after the mouse was bitten, it
was weighed again. He found the snakes injected only a small portion of their
venom when biting the mouse, and if the snake was presented with a second
mouse, about the same amount of venom was injected. It was only after one snake
had bitten nine mice that the amount of venom injected declined, and was completely
expended after 23 bites. In 20% of the bites, Kochva’s snakes injected no
venom. It is this study and similar ones that suggest snakes may meter their
venom.
David
Cundall used videotape to study the viper’s strike; slowing down the motion of a
striking snake make the more subtle and rapid changes visible. He found snakes
did not open their mouths to the maximum extent during the strike. Instead,
maximum gape was obtained only when the snake released the prey. The wide,
elongated head, narrow anterior body, and the enlarged posterior body are
typical morphology for vipers. The head and body shape allows vipers to feed on
prey large in both circumference and mass. Because of this shape, most of the
viper’s mass is located toward the rear of the body, and Cundall suggested this
is needed to anchor the rear body, allowing the snake to accelerate its head
and forebody during the strike. Head acceleration may be fast enough during the
strike that the snake is unable to stop exactly when the prey is reached;
therefore the snake may carry or knock the prey a short distance past its
original position. Vipers may maximize body mass by retaining waste material in
their large intestine to increase inertia so the rear body stays in-place
during the strike and to reduce the momentum of the accelerating head.
In
a review of factors that influence venom expenditure, William Hayes and
colleagues explored whether the amount of venom used during a bite is selected
by both intrinsic and extrinsic factors. They suggested that the amount of venom
needed to subdue or kill prey, alter the odor of the prey so that it can be
trailed after being released, start digestion, and repel predators is
controlled by the snake. With every strike, the venom volume is selected by the
snake for the situation at hand. The proposal suggested the amount of venom
needed to obtain prey may be more than the amount of venom needed for defense,
and that factors such as hunger, size, and species of prey all contributed to
the decision the snake makes about how much venom to release during a bite. According
to the authors, the volume of venom expended by a single predatory bite on an
adult mouse by elapid snakes ranged from zero to 109 milligrams (mg). The Death
Adder injected the most (3–109 mg) venom and the Australian Brown Snake
injected the least (0–10 mg). Eight species of vipers were tested and the
Palestinian Viper injected the most (1–188 mg), and the Russell’s Viper
injected the least (1.2–2.4 mg). The amount of venom injected is always a
fraction of the venom available, and varies from about 12% in the Russell’s Viper
to 50% in the death adder. Elapids tend to inject more of their venom than
vipers, and Hayes and colleagues suggest this was related to elapids biting and
holding their prey. Vipers usually employ the bite-and-release strategy.
Fang Behavior
Another
window to understanding the nature of snakebites is the behavior of the fangs
before and during contact with the prey.
Keeping in mind that viper fangs [Figure 6–1] are long, mobile, function
independently of one another, and that the snake is attempting to sink at least
one of the fangs into a live, moving animal makes for a complex problem for
both the snake and the scientist trying to understand the events.
INSERT
FIGURE 6-1.
Figure 6–1. A: A Terciopelo (Bothrops
asper) having its venom extracted. The fang sheath is visible. B: An
Indo-Chinese Spitting Cobra (Naja siamensis) and venom.
In
a more extensive study than his previous one, David Cundall videotaped more
than 750 strikes from 285 vipers of 86 different species. Viper strikes are
relatively fast. According to the results of the study, mean time for the snake
to gape its mouth was 80 milliseconds (ms). Cundall found vipers usually
contact the prey first with the lower jaw and then close the mouth to drive the
fangs into the prey’s tissues. As the fang penetrates the prey, the sheath
slides up the fang. Bites that did not involve fang repositioning had an
average duration of 140 ms. Repositioning fangs after they had made contact
with the prey occurred in 39% of the strikes, and the bite time increased to an
average of 185 ms. Fangs for the species Cundall examined were 3–35% of the
mandible length. The distance from the upper edge of the venom discharge
opening to the tip of the fang ranged between 12–51% of the fang’s total length.
Interestingly, species with shorter fangs had longer discharge openings.
Cundall, and previous researchers, suggested viper fangs are long as an
adaptation to feeding on vertebrates. A fang sinking into a vertebrate may
encounter bone or solid connective tissue which would prevent the fang’s
discharge orifice from extending below the skin, keeping the venom from being
delivered into the prey. However, venom expulsion from a fang not embedded in
prey is not common, suggesting the snake has some feedback about the position
of the tooth. A likely source for this feedback is the position of the fang’s
sheath, something already found to play a role in venom flow. A better position for the fang’s discharge
orifice might be at the tip of the fang, just as the discharge opening for a
hypodermic needle is at the tip of the needle. This condition has not evolved
in vipers or other front-fanged snakes, and the reason may lie in the way the
fang develops or the mechanical properties of dentine and enamel. It may also
be that soft tissue would plug the opening more readily and not let venom
escape the fang into the prey. All of the evidence Cundall found suggested
snakes have incredibly fine neural control over the strike and bite. Snakes are
not working from sets of pre-programmed instructions but are adjusting their
movements for the situation by the millisecond.
Cundall’s
study examined viper fangs capable of folding back into the roof of the mouth
on a rotating maxillary bone, making it possible for the snake to reposition
the fangs during the strike. The elapid maxillary bone and fangs are far less
adjustable and, therefore, the fangs and the maxillary are better adapted to
holding prey in the snake’s mouth.
Venom Metering
The
unpredictable nature of snakebites, the substantial number of dry bites, the
fact that empty venom glands may take days to weeks to refill, the idea that
venom may be expensive for the snake to produce, and the studies showing the
volume of venom injected during a bite was highly variable all lead
herpetologists to speculate that snakes are making decisions on how much venom
needs to be injected in a given situation. Sherman and Madge Minton wrote,
Our observations on the feeding of captive
venomous snakes of many kinds over a period of more than thirty years have
convinced us that snakes can size up their prey and gauge their attack
accordingly; moreover, there is a difference between a defensive strike and one
intended to kill.
The idea that snakes meter their venom and
have control over the volume of venom they inject has become well accepted.
Considering the strike of a viper is often 50 to 200 ms in duration and there
is no obvious way to observe venom flow, it is difficult to find evidence for
or against this hypothesis, but not impossible.
Measuring
the volume of venom injected during a strike can be achieved by ELISA
(enzyme-linked immunosorbent assays), a biochemical tool developed in the
1960's to detect the presence of an antibody or an antigen in a tissue sample.
ELISA is useful in medicine and other research that involves antigen-antibody
reactions. ELISA has been adapted for detecting venom in potential snakebite
victims. The test is particularly useful when a person has been bitten by a
snake but was not aware of the bite or is not capable of communicating with a
physician, as is often the case with young children or unconscious adults. Antigen
protein molecules are attached to a surface (usually a plastic microliter
plate), and then washed with a specific antibody so the antigen can bind to its
surface. An enzyme is linked to the antigen, followed by the addition of a
signal substance that attaches to the enzyme and can be detected. The signal
can be a molecule that is radioactive, fluoresces, or changes color when light
of a specific wavelength illuminates the plate. The strength of the signal
allows the volume of venom to be determined.
The
first use of an early ELISA-type test used to detect venom was in 2-year-old
Belinda Smith of Jandacot, Western Australia. Belinda was seen playing with a
piece of orange rope and soon after complained of having been bitten. Four
puncture marks were present on her arm and her mother cleaned the wounds.
Within minutes Belinda began to vomit; her father searched for the rope but did
not find it, and she was taken to the hospital. She was kept for two hours and
released after she showed no signs of envenomation. Her mother put her to bed
and monitored her throughout the night. At 7:30 AM the next morning she was
comatose, and at 8 AM she was pronounced dead at the hospital. Blood and
tissues were sent to the Commonwealth Serum Lab in Melbourne, Australia where
the tissues were examined with a radioisotope test. The cause of Belinda’s
death was Tiger Snake (Notechis scutatus) venom.
William
Hayes and colleagues used ELISA to measure the quantity of venom injected into
mice by the Northern Pacific Rattlesnake (Crotalus oreganus) in order to study
venom metering. Medium and large-sized snakes injected similar quantities of
venom, but they found the snakes injected more venom into larger prey. In
addition to measuring the venom volume, they videotaped the snakes’ strike and
found no behavioral differences that corresponded to the quantity of venom
injected. Their conclusion was that the venom expended was the result of
intrinsic control of venom flow.
In
a critique of the venom metering hypothesis, Bruce Young and colleagues note that
the venom doses injected are often several times the lethal dose, and the
snake’s ability to assess the nature of the target during the strike is
questionable given the short duration. Additionally, they point out that
hypothesis relies on the snake’s abililty to control the venom apparatus,
something they suggest may not be possible. Fine control of muscles on the
gland’s compartments, and the control of venom flow through the venom duct and
associated structures, would be necessary. If the venom apparatus exerts a
variable influence on venom expulsion then the metering hypothesis seems
unlikely.
Young
and colleagues pointed to the dry bite phenomena as evidence of this. Dry bites
could occur because the snake decided not to inject venom, or because the
activation of the venom apparatus failed for a number of different reasons.
Alternatively, they proposed the pressure-balance hypothesis to account for the
variation in venom doses delivered during a bite. This idea depends on three
factors: (1) the pressure placed on the venom gland by the attached muscles, (2)
the pressure in the chambers near the fang (the duct, venom vestibule, venom
chamber, and the entrance opening to the fang) and (3) the resistance of venom
leaving the fang tip once it has sunk into the prey.
Pressurized
venom leaves the gland, flows through the duct and enters the venom vestibule,
the venom chamber, and the opening of the fang canal where venom runs through
the fang’s canal to the exit opening near the fang’s tip. Once the fang’s tip
is embedded in the prey, the tissue of the prey surrounds the fang’s opening
and offers resistance to the venom attempting to flow out. However, the amount
of resistance depends on the kind of tissue. For instance, if the fang
penetrates a muscle the resistance will be greater than if it hits the center
of a blood vessel. If the resistance in the prey’s tissue is greater, then more
venom can be expected to be found on the prey’s skin because the venom will
leak out of the soft sheath tissue surrounding the fang, and some venom may
actually flow backward into the gland, an event that has been experimentally documented.
In
order to test the pressure-balance hypothesis, Young and Kenneth Kardong examined
the flow of venom in live Western Diamondback Rattlesnakes (Crotalus atrox).
The snakes were outfitted with devices to contract the venom gland muscles and
measure venom pressure at various points along the front end of the venom
tract. Results showed the contraction of the compressor gland muscle accounted
for only 30% of the variation in venom flow. However, when the fang sheath was
lifted, as occurs during a normal strike, the venom flow increased more than 10
times the rate produced by the compressor gland muscle alone. Sliding the
sheath back to expose the fang appears to tighten the tissue, possibly decreasing
the size of the venom vestibule (the expansion of the venom duct near the fang)
and creates a more direct and open route for the venom to flow from the venom
gland to the opening on the fang’s tip.
William
Hayes argues that evidence for venom metering is compelling with the strongest
evidence coming from studies that measure the volume of venom expended during bites
of prey of different sizes. In other words, snakes tend to inject more venom
into larger prey. Also, snakes biting mouse models that lacked a mouse odor
tend have mechanically flawed strikes, probably because the snake did not
detect the chemical signature of the mouse. Mouse models with mouse odor
elicited more mechanically precise strikes.
A
recent study using the Black-necked Spitting Cobra (Naja nigricollis) suggests
that snakes do, in fact, meter their venom. Hayes and co-workers videotaped
defensive bites of this cobra during venom extraction. The snakes bit a piece
of parafilm covering a glass funnel, no pressure was applied to the glands, the
bites were voluntary, and the pulses of venom were timed. The venom was then collected
and weighed. Mean venom flow lasted 0.35 seconds and the mean mass of venom
expended per pulse was 14.2 mg for juveniles and 188 mg for adults. The video was
reviewed and each venom pulse was found to be a discrete event with jaw
contractions followed by a venom pulse. They found this cobra expended four
times more venom when biting than when spitting.
It
seems likely snakes genuinely may be metering venom and that the factors
described in the pressure balance hypothesis certainly play a role in venom
delivery. The two hypotheses are not mutually exclusive and, as more work is
done, more snakes will be shown to have some level of control, possibly a very
fine level of control, over venom expulsion.
The Global Snakebite Problem
Snakebites
are a relatively rare medical hazard for the developed world; but in much of
the rural tropical and subtropical regions, snakebites remains an important
public health problem. A recent study of the global snakebite burden, funded by
the World Health Organization (WHO) and authored by Anuradhani Kasturiratne and
colleagues, estimated the number of envenomations per year between 0.4–1.8
million, with deaths estimated between 20,000 and 94,000. To put this in
perspective, the WHO’s low estimate of snakebite envenomations works out to
1150 people per day, while their high estimate would mean that more than 5000
people per day are envenomated, and 54–275 people die each day from snake
envenomation.
The
WHO’s numbers have come under considerable criticism in part because their
numbers for snakebites in India and Pakistan were so much lower than those of
the previous estimates by Jean-Philippe Chippaux. Chippaux suggested 5.4 million
snakebites annually, with 2.6 million envenomations (or 7100 envenomations per
day), and 125,000 deaths per annum (or 342 people per day die from snake
venom).
There
are 227 countries. The WHO study found 58 of these countries do not have any
incidence of venomous snakebite. These countries include Greenland, Iceland,
Ireland, New Zealand, Madagascar, Cuba, and most of the island nations of the
Caribbean and remote Pacific. These are countries that have no native
front-fanged venomous snakes. The WHO found data for 77 countries with
incidents of snakebite and was able to generate estimates for 92 countries. But
snakebites, as well as other public health issues, remain poorly reported in
many nations.
A
summary of snakebites by country follows. Not all countries are discussed, but
the statistics are based on a review of Chippaux’s book and the recent WHO
paper, as well as other documents. Additional discussion comes from a variety
of sources that can be found in the References and Notes section for this
chapter.
Snakebites
resulting in envenomation on the African continent are estimated to be 100,000,
and there are about 20,000–30,000 deaths annually. Delayed treatment is a
serious problem, with some victims not receiving treatment for one to two weeks
after the bite. In North Africa, the snakebite problem is low, with 15
envenomations per 100,000 inhabitants. Sub-Saharan Africa has many more
venomous snakes, and evidence suggests the snakebite problem is severely under
reported. Many of the envenomations are from the Puff Adder (Bitis arietans)
and two cobras (Naja nigricollis and N. mossambica). Surveys of households in
Nigeria and Kenya report that only 8.5% and 27% of snakebites, respectively,
received hospital treatment, but 70% of the reported bites are likely from
harmless snakes. Several locations in
Sub-Saharan Africa are notable for snakebites.
The southern Ivory Coast has 200–400 envenomations per 100,000
inhabitants; however, among industrial agricultural workers, bites are 3,000
per 100,000 inhabitants. In north Benin, there are 210–650 cases per 100,000
inhabitants and among sugarcane workers, the incident of snakebite is 1,300 per
100,000, deaths are low at 1.5% of envenomations. However, the largest number
of deaths seems to occur in the Benue Valley of Nigeria where snakebite cases
are 600 per 100,000, and death occurs in about 15% of the cases. Most of the
victims are males engaged in agriculture or hunting.
Two species of saw-scaled vipers (Echis
ocellatus and E. leucogaster) are probably responsible for 90% of the bites in Nigeria.
Symptoms include localized swelling, blistering, non-clotting blood,
spontaneous systemic bleeding, and necrosis. And, while the bites may causes
death, particularly from excessive bleeding, they more often result in long-term
or permanent disabilities.
In North America there are about 4,735 envenomations
annually; the total number of deaths is about 28 per year. Of the bites, 98%
were from vipers and 2% from elapids. About 77% of victims were male, 70% were adults
20 years old, or older, and 12% were less than 10 years old. There were 65 cases involving pregnant women
bitten by rattlesnakes, and 70% of them resulted in moderate-to-severe effects.
Rattlesnakes and copperheads produced the most severe results in children less
than six years of age.
A survey of 142 snakebite fatalities that
occurred between 1979 and 2005 found 90% of the bites were from native pitvipers,
2% from native coral snakes, and 8% from exotic species (mostly tropical
American pitvipers of the genus Bothrops, African vipers of the genus Bitis and
Asian cobras of the genus Naja). Fatal
bites were sustained mostly by males (80%) who were Caucasians (94%), between
the ages of 25–54 (52%) and many were intoxicated while handling the snake. Geographically,
55% of the fatalities were in the states of Texas, Georgia, Florida, Arizona,
and California. In a sub-sample of 26 fatal cases with details, 70% of the
bites were from rattlesnakes, 19% were from exotic snakes, and 7 of the 26
(27%) were bites sustained during religious ceremonies in Appalachia.
Coral
snake bites are relatively rare in the USA and 50–70% of them occur while the
snake is being handled; in some instances the snakes were misidentified, the
handler believing they were harmless mimics. Rob ert
Norris and colleagues report the first documented death from a coral snake bite
in the USA in 40 years. The circumstances of the bite are of interest because
they are representative what happens in many North American envenomations.
On
the June 10, 2006, victim A was drinking alcohol in a wooded area of Lee
County, Florida with friends. An unlucky coral snake crawled into the midst of
the men, and victim B grabbed the snake and was bitten. Victim A tried to stab
and cut the snake with a broken beer bottle and was bitten at least once. The
snake was killed and placed in a milk carton by victim B who rode a bicycle to
a fire station for help. Victim B was taken to a hospital while victim A
continued to drink alcohol. Two hours later, victim A stopped breathing and was
pronounced dead when emergency personnel arrived. Victim B recovered
completely. Victim A’s blood serum was later tested using ELISA and was
confirmed to contain Eastern Coral Snake (Micrurus fulvius) venom. (Here, it is
very difficult to resist making a comment about the Darwin Awards.)
Only
four West Indian islands have venomous snakes (St. Lucia, Martinique, Trinidad
and Aruba) and the WHO study estimated between 1,098 and 8,039 envenomations
per year for the Caribbean. Each of these islands has one or two species of
endemic pitvipers, and Trinidad has two species of coral snakes.
In
Central and South America snakebite frequency is much higher, in part due to
the greater diversity of pitvipers. Total bites in Latin America are estimated
at 300,000 and there are about 5,000 deaths per year. Mexico is estimated to
have 28,000 envenomations per year with about 1000 deaths. Snakebites may be
severely under reported in Mexico considering the high numbers of rural poor
who do not use hospitals. The rich
diversity of pitvipers and coral snakes in Mexico were a problem for the anacient
Maya as they are for the present-day citizens. The lanceheads of the genus
Bothrops have venom with hemorrhagic action, properties that the Maya were well
aware of. R. L. Roys translated a Maya
passage that stated, “…when it bites a person, it causes him to exude blood
from every pore like a bloody sweat, and if no remedy is applied, he will die
in a day…”
Costa
Rica has about 1,000 envenomations each year, with 30 to 40 deaths. Most deaths
are young males between 10 and 19 years old. Fatalities have declined from 5
per 100,000 in 1952 to 0.15 per 100,000 in 1996. By the 1990’s, Costa Rica’s
population had increased and the annual number of snakebites increased to an
average of 504 envenomations per year. However, the incidence per 100,000
people declined. Agricultural workers are most susceptible, and the snake of
most concern is the Terciopelo (Bothrops asper).
Brazil
has an estimated 25,000 envenomations, (roughly 200 per 100,000) and the death
rate is low at about 0.4 to 5 per 100,000 residents, but the state of Amazonas
has 350–450 bites per 100,000 residents. In the dry, northeastern part of the
country, lanceheads (Bothrops) are responsible for most (56%) of the bites; 32%
were from rattlesnakes (Crotalus) and 1% from the bushmaster (Lachesis). In the
Mato Grosso, 99% of 307 cases documented between 1993–95 were from lanceheads.
A survey of households in Amazonas suggested snakebites were six times more
common than official reports would suggest, however, many of these may be from
non-venomous, or mildly venomous species.
In
Columbia, about 2,700 snakebites were reported annually during the 1990’s and
the frequency was 23–26 bites per 100,000 residents. Lanceheads (Bothrops) were
responsible for 95% of the bites and the fatality rate was about 5%.
In
Ecuador, about 4,000 people are hospitalized for snakebites, about 200 (5%) die.
Among indigenous peoples living in forest, however, the bite frequency may
reach 1,000 per 100,000 annually.
In
French Guyana, 110–120 people are hospitalized with envenomation and deaths
number two or three per year. However, some locations may have bite frequencies
that reach 590 per 100,000 residents.
Asia
has the highest incidence of snakebites, as a result of its dense population
and diverse venomous snake fauna. An estimated 2 million envenomations and
100,000 deaths occur per year (about 274 deaths per day).
Information
on snakebites in China is scant, despite a fauna that contains numerous elapids
and vipers. A 1990 report mentions 1,427 bites from the Short-tailed Mamushi (Gloydius
brevicaudus) with one fatality. And, 120 cases of Chinese Moccasin (Deinagkistrodon
acutus) bites with two fatalities, 31 disabilities, and 87 complete recoveries were
reported in one paper. The reason for China’s poor snakebite data is discussed
below. However, a recent paper by Wong Oi-Fung and colleagues surveyed four
Hong Kong snake shops to identify species that may be involved in snakebite
incidents. Expecting to find the four local species (the White-lipped Pitviper,
the Chinese Cobra, and two species of local kraits), the team was surprised to
find that local species were in short supply and that shops were importing
snakes from Thailand. Snakes that were found in Hong Kong’s shops included the
Monocellate Cobra (Naja kaouthia) and the Hamadryad (Ophiophagus hannah). The
Hamadryad is known from Hong Kong, but they are considered rare on the island.
Their presence in the snake shops suggests they were also imported, probably
from Thailand. Another likely Thai import, the Red-necked Keelback (Rabdophis
subminiatus), was also being sold in the snake shops, and it, too, could pose a
significant health hazard.
Japan
has a relatively low overall incidence of snakebites (1 per 100,000 inhabitants).
But, the southern archipelagos are tropical, and some islands have an incidence
of snakebite that approach 600 per 100,000. The Amami Islands of Japan were
covered with forests until they were colonized by humans who cleared the trees
for agricultural crops like sugar cane and hay. People living here were at
great risk of being bitten by a large (1.8 meter) venomous snake, the Habu (Protobothrops
flavoviridis). The death rate from the bite of this pitviper was 10–15% of the
envenomations prior to the start of the 20th century. However, the first
antivenin was developed for Habu bites by 1905, and the death rate declined.
Unfortunately, the bites still did major damage to the victims via necrosis. Necrosis
occurs as venom enzymes digest their way through the tissue, turning body parts
to liquid that will not regenerate. Necrosis from Habu venom has left many
Amami farmers crippled and disfigured.
By
the 1960’s, the Habu became the subject of intense study by Japanese
scientists. During this decade, an average of 250 people were bitten each year,
and the maximum number of bites in a single year could be as high as 600 per
100,000 people in the areas of highest risk. The studies revealed that the
larger the area under cultivation, and the greater the number farmers, the
higher the incidence of snakebites. Most of the bites took place when farmers
were working in their fields, harvesting sugar cane or weeding, though some
bites occurred around houses and along roadsides. Most bites occurred during
the day even though the Habu is nocturnal, presumably because farmers disturbed
the snakes in their daytime hiding places.
Science’s
war on reducing the number of Habu bites took many paths. The use of antivenin
was helpful, but could only be used after the bite occurred. People still
suffered the effects until they could get the serum. The production of a
vaccine or toxoid was an attempt to be proactive, making the farmers resistant
to the venom. Habu venom was treated with acid to deactivate its enzymes. Farmers
were then inoculated with the toxoid, allowing their bodies to build resistance
to necrosis. The vaccine was somewhat successful. The third step was to remove
as many Habu from the farm fields as possible, reducing human contact with the
snake. This was accomplished with electrified fences that kept snakes out of
fields, as well as collecting snakes with baited traps. The added steps of
keeping fields and yards free of rats, training dogs to find snakes, and hiring
people to catch Habu, met with mixed results. Today Habu are still a threat to
the farmers of the Amami Islands, although the risk may be less than it was 50
years ago.
South
Asia (Bangladesh, Myanmar, Nepal, Pakistan, Burma, India, Sri Lanka) has the
most snake envenomations of any region in the world, at 121,000 per year, and
the highest number of deaths due to snakebite, estimated at 14,000 annually.
This works out to more than 331 people per day who are envenomated by snakes,
and 38 deaths per day.
Snakebites
in Bangladesh are poorly known. A 1988–89 survey of 10% of the country
suggested there were 764 bites reported in a single year, with 168 deaths
(22%). Cobras were responsible for 34% of bites and these had a 40% fatality
rate.
India
has the highest incidence of snakebites. Reports have estimated as many as 200,000
bites and 50,000 deaths annually. But these numbers are likely inflated.
Chippaux suggested it is 65–165 per 100,000 inhabitants using data from areas
with the highest snakebite numbers, with about 70 envenomations per 100,000
residents. The WHO estimated that envenomations exceed 100,000 per year, and
deaths exceed 11,000 per year. While the number of bites is low per 100,000
individuals, the actual number of people envenomated by snakes in India is higher
than any other country, with an estimated 81,000 envenomations yearly. People
treated in a hospital have a 1.5–20% death rate. Most bites occur between June
and November, and bites from vipers are twice as common as bites from elapids.
But the death rate from vipers is about 6% and death from elapids is 25%. The
WHO numbers for Indian snakebites are much lower than those reported by earlier
studies. Four species of cobras (Naja), at least four species of kraits (Bungarus),
Russell’s Viper (Daboia russelii), two species of saw-scaled vipers (Echis),
and the Humped-nosed Viper (Hypnale hypnale) are the species responsible for
envenomations. All of these snakes seem to thrive in human-modified habitats,
feeding on rodents, and using microhabitats created by agriculture and
urbanization.
Myanmar
(Burma) has between 35 and 200 bites per 100,000 residents, not a particularly
high incidence, but it has the highest death rate at 35 deaths per 100,000
envenomations. The Russell’s Viper
(Daboia russelii) is thought to be responsible for 90% of the cases. The
numbers reported are probably low; in 1991 there were an estimated 14,000
envenomations or bites with 1,000 fatalities, and there were more than 8000
bites with 500 fatalities in 1997. Bites peak in May and June in urban areas
and during the rice harvest from October to December in rural areas.
Nepal
is estimated to have 20,000 bites per year and more than 1,000 reported deaths
with most of the bites occurring during the monsoon season. Nepal may rank
fourth in the world for the most envenomations. About half of the bites are
from snakes not identified, but 30% are from cobras (Naja and Ophiophagus),
16.7% from kraits (Bungarus), and 3.3% from the green pitvipers (Trimeresurus
complex). Many victims show signs of neurotoxins with drooping eyelids, slurred
speech, and respiratory distress. Of 290 cases reported by hospitals between
1989 and 1995, there were 175 fatalities (60%).
Envenomations
in Pakistan are estimated at 12,000 per year with deaths estimated at 1200 per
year, most of which occur in the agricultural areas of Sindh. The common Indian
Cobra (Naja naja), Russell’s Viper (Daboia russelii), and the Indian Krait
(Bungarus caeruleus) are responsible for some of the bites, but the Northern
Saw-scaled Viper (Echis sochureki) is the species responsible for most of the
bites and deaths.
The
densely populated island nation of Sri Lanka has about 250 bites per 100,000
inhabitants. The Indian Cobra (Naja naja) and Russell’s Viper are responsible
for 35% and 40% of the bites, respectively. Total annual envenomations in Sri
Lanka are estimated at 33,000 in the WHO study, but some of the same authors
published a study in 2004 stating envenomations in Sri Lanka numbered 14,000 per
annum. Sri Lanka is second in the list of countries with the most
envenomations.
Southeast
Asia is right behind South Asia with 111,000 envenomations per year, or an
average of 304 envenomations per day. However, many countries with large
populations such as Cambodia, Laos, and Indonesia numerous venomous snakes lack
snakebite statistics.
In
peninsular Malaysia snakebite data is not collected, but bites are thought to
be common, particularly in the north near its border with Thailand. Malaysia
and other countries may not collect snakebite data because of the cultural
beliefs of the population. H. Alistair Reid, a physician at Penang’s General
Hospital, made more than 50 visits to 17 villages in the northwest peninsula to
determine the incidents of sea snakes bites, discover how the victims were
bitten, and determine the survival rate. Carrying a bag of dead sea snakes and
accompanied by a health worker known to the local fishermen he visited coffee
shops. Reid started the conversation by opening the bag. The snakes attracted
much interest until the subject of bites was brought up. People became less
talkative, wandered off, and denied all knowledge of bites. All deaths must be
reported to the police, and a snakebite death is considered sudden. This requires
a doctor viewing the body and increases the probability that the body will be
removed, the burial delayed, and a postmortem performed. The Malay and Chinese
are offended by these procedures and snakebite deaths were often attributed to
a "fever," or some other problem that would be accepted by local
officials.
Reid’s
investigation found 144 cases, 25 (17%) of which were fatal. Of the 144 cases,
only 18 sought hospital or dispensary care, and six of these were fatal. Reid
considered these cases to be a gross underestimate of the actual number of
bites that occur. The diagnosis was not always certain, and it was known that
some died who did not go to the hospital; the mortality rate was somewhere
between 3% and 25% for sea snake bites untreated by specific therapy. Reid
investigated 120 cases of sea snake bites, and found 41% happened while fishers
untangled nets with trapped snakes. Other bites occurred while sorting fish or
wading in water. Reid sampled 600 sea snakes (alive and dead) during the study.
Of these, 158 of these were the Beaked Sea Snake (Enhydrina schistosa), 178
were the Curtus’ Sea Snake (Lapemis curtus), and 101 were the Annulated Sea
Snake (Hydrophis cyanocinctus), and all were species most likely responsible
for the bites.
From
1958 to 1980, there were 55,000 snakebites reported in Malaysian hospitals.
Based upon these numbers, the mortality rate is only 0.3 per 100,000 individuals,
but the local necrotic effects of some venoms can cause prolonged morbidity and
crippling deformities. Although the Malayan Pitviper (Calloselasma rhodostoma)
was responsible for most of the bites, the numbers may be severely under
reported for the reasons suggested by Reid.
Thailand
has more than 10,000 envenomations each year with the Malayan Pitviper responsible
for 35–40% of the bites. In 1989, there were 6,038 bites reported with 19
deaths. About 2% of the bites were fatal. The green pitvipers (Trimeresurus complex)
accounted for another 25–30% of the bites and while fatalities are known, they
are rare. Russell’s Viper accounts for another 15% of bites; this snake is particularly
common in Thailand’s Central Plain and has a very low mouse LD50 (about 1.6
micrograms). A lethal human dose ranges from about 20–25 milligrams. In 46
fatal cases, Malayan Kraits (Bungarus candidus) and the Malayan Pitviper were
each responsible for 13, the Monocellate Cobra (Naja kaouthia) was responsible
for 12, and Russell’s Viper for seven deaths. Snakebite deaths in Thailand have
been greatly reduced with the availability and use of antivenom. In 2004, I
visited a snakebite clinic in southern Thailand that continued to use
traditional herbal remedies for snakebites. Rubber plantations were common in
the area, and rubber tappers are susceptible to snakebites as they often walk barefoot
from tree to tree.
Vietnam
has 30,000 envenomations per year, placing it third on the list of countries
with the most envenomations where it is tied with Brazil. Again, the snake responsible for most bites
is the Malayan Pitviper but cobras and sea snakes are also likely to be
involved.
Rice
farmers in the Philippines have exceptionally high snakebite mortality, but the
numbers are rough estimates. George Watt and colleagues from the U.S. Naval
Medical Research Unit No. 2 suggested deaths from cobra bites may be as high as
107 per 100,000 residents and confirmed a death rate of 53.8 per 100,000
residents. They found only 8% of the victims studied survived to reach the
hospital. An estimated 200 to 300 deaths per year from cobras (Naja sp.) are suspected.
The
island nation of Taiwan has about 15,000 to 20,000 bites per year and about 500
deaths per year from snakebite. The snakes most often responsible include Stejneger’s
Green Pitviper (Trimeresurus stejnegeri), Russell’s Viper (Daboia russelii),
cobras (Naja), and the Taiwan Habu (Protobothrops mucrosquamatus).
Australia
is well known for its highly venomous snake fauna, with most snake species
belonging to the front fanged Elapidae. The island continent has 1,000–3,000
snakebites per year with the number of bites decreasing in the temperate
regions. This has been attributed to urbanization and lifestyle changes with
more people living in cities. But, the introduction of the poisonous Marine
Toad (AKA the cane toad) has also been implicated in reducing the number of
frog-eating snakes. Additionally, the increased use of fertilizers and
pesticides in agricultural regions has reduced the food supply for snakes, and
these chemicals may play a role in poisoning or disrupting their physiology.
In
1940, Hugo Fleckner discovered tropical Queensland had more snakebites than
southeastern subtropical areas of the state, even though the tropical region of
the state had only one-third of the population found in subtropical regions.
Children in subtropical southeast Queensland had a snakebite frequency of 7.1
per 100,000 in the early 1970’s. Bart Currie found the annual rate in the
1990’s of snakebite in children was 18.3 per 100,000 in the Northern Territory,
but notes that it decreased to 4.0 per 100,000 by 1998. Deaths from snakebite
are now rare in Australia. No deaths from snakebite in the Northern Territory
occurred in the 1990’s despite the state having the highest rate of snakebite
incidents in Australia. With the discovery and availability of antivenom at the
start of the 20th century, the mortality dropped from 13 per year in 1900 to
less than four per year by the late 1970’s.
Snakes
responsible for bites in the Northern Territory are, in decreasing order of
importance, the Western Brown Snake (Pseudonaja nuchalis), the Mulga
(Pseudechis australis), the Death Adder (Acanthophis antarcticus), and the Coastal
Taipan (Oxyuranus scutellatus). In tropical Queensland the Eastern Brown Snake
(Pseudonaja textilis), the Coastal Taipan, Western Brown Snake, the Mulga,
Death Adder, Rough-scaled Snake (Tropidechis carinatus), and Eastern Small-eyed
Snake (Cryptophis nigrescens) delivered the most bites. Recent estimates for
the number of deaths across Australia from venomous snakes are six per year, and
anecdotal reports suggest death from snakebite was more common in 19th century
Queensland. Garde, writing about Queensland snakebites, reported that a Mr.
Jonstone from northern Queensland had seen four out of seven people bitten by
death adders recover, but he had attended funerals of all 12 people who had
been bitten by the "brown snake" or taipan. Prior to the availability
of antivenom, only two people were known to have survived taipan bites.
Snakebites
in New Guinea are a different story. The coastal Kairuku area just north of
Port Moresby (Papua) had a snakebite incidence of 526 bites per 100,000; a
frequency close to the highest reported in the world. Papua is tropical, so snakes
are active and biting year-round. The snakes responsible for these bites are
the Papuan Taipan (Oxyuranus scutellatus canni), death adder (Acanthophis sp.),
Papuan Black Snake (Pseudechis papuanus), the New Guinea Small-eyed Snake
(Micropechis ikaheka), and the Brown Snake (Pseudonaja sp.). The estimated number
of deaths per year for the entire island of New Guinea is estimated to be 22
per 100,000. In the mid 20th century, snakebites were thought to be responsible
for 155 hospital admission per year, 6.3 per 1,000 admissions in Papuan
hospitals. Overall Australasia is estimated to have 1460–5895 envenomings per
year, with annual deaths estimated at 229–520. Since the number of deaths in
Australia is less than 10 per year, it is clear most bites occur in New Guinea.
Effects of Venom
Venoms
have traditionally been classified as neurotoxic or hemorrhagic, with elapid
venoms having mostly neurotoxic symptoms and viper venoms damaging blood
vessels and altering blood clotting mechanisms.
Terrestrial elapid venom (African cobras, coral snakes, mambas, and
kraits) is often described as doing little damage at the bite site. Instead,
these venoms have a systemic impact the nervous system. However, the exceptions
are quite numerous. The African Black-necked Cobra (Naja nigricollis) and the
Mozambique Spitting Cobra (N. mossambica) cause significant swelling and local
damage from necrosis at the site of the bite and produce virtually no
neurotoxic symptoms. The cobra that may damage tissue to the greatest extent is
the South African spitting Rinkhal (Hemachatus heamachatus). This snake has low
viscosity venom, making it easier to spray; while its venom has relatively low
toxicity it causes considerable tissue damage. Tissue is liquefied as the
enzymes break cell membranes and digest the adhesive that cements cells
together. These cobras rarely cause damage to nerves. On the other hand, some
rattlesnakes have been shown to have potent neurotoxic venom (see Chapter 5).
Neurotoxic
envenomation first impacts muscles well supplied with nerves like the upper
eyelid, eye ball muscles, and muscles on the lens of the eye. Twenty minutes to
several hours after being bitten, the victim will likely have dropping eyelids,
blurred vision, headache, and excessive drooling. Paralysis sets in and
eventually moving the jaw, talking and breathing become impossible. Once
breathing stops, death can only be postponed with the use of artificial
respiration devices or rescue breathing. The krait -suffered by Slowinski
demonstrated these kinds of symptoms. Toxins in these snakes interfere with the
ability of nerve cells to pass their message to the muscle cells.
Neurotoxic
venoms, like those found in cobras, may act post-synaptically by blocking the
receptors of acetylcholine; or they may act before the synapse (pre-synaptically)
by destroying the vesicle at the end of the neuron that produces the
acetylcholine, as found in kraits. Pre-synaptic venoms are more serious because
the neurons have to rebuild the vesicles, and this may require the victim to be
on a ventilator for days or weeks while their body repairs the damage. The
pre-synaptic venoms cause massive paralysis and may give the impression that
the patient has died when they are in-fact, completely conscious and aware of
what is going on around them but unable to respond because of the paralysis. Post-synaptic
venoms can be cleared from the receptors relatively easily within hours or a
day or two, given the help of antivenom.
Australian
elapid venoms produce many different symptoms depending upon the species. Brown
snakes (Pseudonaja) alter the clotting ability of blood. Tiger snakes (Notechis)
and taipans (Oxyuranus) cause swelling, lower blood pressure, damage muscles,
produce convulsions, and damage kidneys.
Death adders (Acanthophis) have severe neurotoxic symptoms that appear
rapidly.
Sea
snakes do bite humans, but frequently deliver dry bites at a rate that may be
as high as 80%. Sea snake venom is painless at the site of the bite, but if
envenomated, muscles stiffen and ache, and spasms begin to occur within minutes
to hours. Headaches, thirst, and vomiting soon follow and three to six hours
after the bite the victim’s urine may start to turn dark from the breakdown of
myoglobin. Sea snake venom is mostly myotoxic, attaching to muscle and damaging
the membranes and neuromuscular junctions. Death may occur more rapidly with a
large dose of venom. The widespread Beaked Sea Snake (Enhydrina schistosa) has
a mouse LD50 of 0.04 mg/kg, suggesting the venom is exceptionally toxic.
Viper
venom often results in swelling, but some species such as the Russell’s Viper
(Daboia russelii), and saw-scaled vipers (Echis) may not cause any swelling
whatsoever [Figure 6–2]. Viper venoms also tend to liquefy tissue, and this may
rapidly spread from the site of the bite and continue for days after the bite,
requiring amputation of a limb. Continuous bleeding from the fang punctures,
eyes, nose, mouth, and anus may occur, while blood may be clotting in other
parts of the body at the same time. The continuous bleeding results from
consumption coagulopathy where the haemorrhagins disrupt the blood’s ability to
clot. Some vipers and rattlesnakes may also induce neurotoxic symptoms, and
viper venoms often have a combination of toxin and enzymes that work in the
blood stream to damage nerve cells and tissues.
INSERT
FIGURE 6-2.
Figure 6–2. Necrosis from the bite of a
saw-scaled viper (Echis). Photo by Ian Simpson.
The African and Middle Eastern stiletto
snakes’ venom cause swelling and work on the blood vessels and heart. They also
liquefy tissues, induce vomiting, and make breathing difficult. Death can occur
in less than 60 minutes. Stiletto snakes produce a unique group of toxins with
neurotoxic, renal, pulmonary, and cardiovascular effects. A researcher bitten
while extracting venom from an Israeli Stiletto Snake (Atractaspis engaddensis)
sustained a puncture from one fang. Swelling,
discoloration, and numbness occurred within minutes of the bite. Systemic
effects soon followed: weakness, sweating, vomiting, diarrhea, fluctuations in
consciousness, and blood pressure increased to 180/110. The victim survived but
discoloration, tenderness, and pain around the site of the bite remained for 10
months.
A
snakebite qualifies as a medical emergency, one that has caused medical
professionals to take desperate measures. While antivenom has gone a long way
toward reducing the need for radical measures, they are still sometimes
necessary. Prior to the option of antivenom, William Theobald writing in 1876
commented on Joseph Fayrer's recommended treatments for snakebite.
...Dr. Fayrer treats this subject
exhaustively in his elegant and valuable work on the Thantophidia, and
recommends such heroic treatment not only as actual cautery with live coals or
gunpowder, or the free use of mineral acids after excision of the bite, but
even amputation of a limb to save a life. Doubtless in the hands of intelligent
medical men such remedies are not altogether condemned, but to recommend such
treatment in general, seems to me to risk subjecting the unhappy sufferer to
fruitless agony at the hands of anxious but wholly ignorant friends, without
the smallest possible chance of any good resulting from such a course.
By the end of the 19th century a much more
efficient, effective, and humane treatment for envenomation was being
developed―antivenom sometimes called antivenin.
Antivenom
The
observation that people infected with a disease did not become re-infected is
ancient and dates to at least 2430 YBP. It was not until the 19th century that
experimentation with snake venom was applied to the concept of immunity. Henry
Sewall, working at the University of Michigan in 1886–1887, used Pigeons and venom
from the Eastern Massasaugua (Sistrusus c. catenatus) to demonstrate that organisms
could be made resistant to rattlesnake venom. Sewall injected small doses that
were gradually increased until the birds could withstand 10 times the lethal
dosage. Sewall’s experiments were the stimulus for developing other antitoxins.
Within
a year, Pierre Roux and Alexander Yersin demonstrated animals could be
immunized to the Diphtheria toxin using the blood from animals exposed to the
toxin. And, in 1890, Emil von Behring and Shibasaburo Kitasato showed passive
immunity for Diphtheria and tetanus, and initiated antiserum therapy. Soon
afterwards these techniques were applied to the snakebite problem.
In
1894, Maurice Kaufmann duplicated Sewall’s results using viper venom. A series
of 1894 experiments done by Césaire-Aguste Phisalix and Gabriel Bertrand at the
Natural History Museum in Paris took the work a step further. They inactivated
the venom by heating it to 68ºC for five minutes and immunized Guinea Pigs against
the venom. Furthermore, they took blood serum from resistant Guinea Pigs, mixed
it with snake venom and gave it to untreated rodents. Resistance to venom was
transferred with the serum. However, their work only produced neutralization of
venom in glassware, not immunization in a living animal.
The
French Colonial Health Service established a daughter organization to Paris’
Pasteur Institute in Saigon, French Indonesia (now Ho Chi Min City, Vietnam) to
produce vaccines for Small Pox and Rabies in 1891. Albert Calmette was
appointed director of the Saigon Institute, and soon after he arrived an
exceptionally heavy monsoon resulted in cobras invading the village of Bac-Lieu.
Forty people had been bitten and at least four deaths occurred immediately. One
of the villagers captured 19 snakes and shipped them to the Pasteur Institute
in a barrel. The snakes were euthanized and their venom glands removed and
stored. Calmette knew of Roux and Yersin’s work with diphtheria toxins, and
that they had produced an antiserum to the toxins that would cure the sick.
However, Calmette’s first attempts to produce a cobra venom cure took a
different path. He experimented with a gold chloride solution which failed to
work after two years of research in Saigon. Ill with dysentery, he returned to
Paris and continued the search for an antiserum. In 1894, he succeeded by
diluting cobra venom with sodium or calcium hypochlorite and subcutaneously
injected rabbits every 8–10 days with an increasing dose. He was eventually able
to inoculate the rabbits with 35 mg of cobra venom with no signs of envenomation. Calmette experimented further and found that rabbits
inoculated with cobra venom that showed signs of envenomation could be cured
with the antiserum.
Calmette’s
success led to a dispute with Phisalix and Bertrand over the priority of the
discovery of antivenom serum, a dispute that fueled a long standing rivalry
between the Paris Museum and the Pasteur Institute. Today, Calmette is credited
as the discoverer of snake antiserum because Phisalix and Bertrand’s reaction
only involved the formation of immunoglobin M, which allowed for the
neutralization of venom. Calmette’s work produced hyperimmunized animals that
produced specific immunoglobin G (IgG) that would protect against envenomation
in a live animal. By the end of 1894, Calmette was using donkeys to produced
anti-cobra serum that could be used to treat humans. In 1896, Calmette became the
Director of the Pasteur Institute in Lille, France, where he produced cobra antivenom
using horses venom supplied from Saigon.
Thomas
Fraser confirmed Calmette’s work and exhibited a rabbit vaccinated against a
dose of cobra venom 50 times the lethal level before the Medico-Chirurgical
Society of Edinburgh. He also used Timber Rattlesnake and Australian Tiger Snake
venoms to produce animals that were immune to each of these species’ venoms.
However, Calmette believed all snakes produced the same venom and claimed his
cobra antivenom effective against a wide range of species, including the
European Adder, the Australian Tiger Snake, and the Australian Black Snake. His
thinking changed by 1904 when he suggested venom came in two forms, neurotoxic
and hemorrhagic.
Vital
Brazil, a Brazilian physician, had worked for a state’s Sanitary Department as
well as maintained a private practice. He had dealt with outbreaks of cholera
and yellow fever, and had the opportunity to work with snakebite victims.
Observations and experiments revealed venom from lanceheads and tropical
rattlesnakes produced different symptoms. In 1896 he read Calmette’s work,
closed his practice, and returned to São Paulo to work with Aldolpho Lutz at
the Institute of Bacteriology. In addition to his normal workload, he began
injecting dogs and goats with small doses of untreated venom from the Tropical
Rattlesnake (Crotalus terrificus) and the Jararaca (Bothrops jararaca). By 1898,
Brazil had evidence that venom was species- specific. Rattlesnake antiserum did
not provide immunity for the lancehead venom and vice versa. He also tested
Calmette’s cobra antiserum against the neurotoxic rattlesnake venom and found
it ineffective. The Institute of Butantan opened in 1901 and Brazil was named
Director. The Institute produced vaccines for the plague, and used horses and
mules to produce snake antivenoms. Some were injected only with tropical
rattlesnake venom, others with a mixture of lancehead venoms (Bothrops atrox,
B. alternatus, and B. jararaca). By
immunizing horses against multiple snake venoms, he was able to produce the
first polyvalent antiserum, a valuable tool for dealing with a snakebite when
the snake could not be identified to species. Brazil distributed antiserum,
syringes, a tool for catching snakes, and wooden boxes for shipping snakes to
the larger plantations and ranches. This gave local people access to medical
treatment and allowed the Institute to obtain more than 5,000 snakes per year,
including many new species. During a visit to New York in 1915, Brazil was
asked to help treat a Bronx Zoo employee bitten by a Western Diamondback Rattlesnake.
The man showed symptoms of severe envenomation and Brazil successfully treated
him with a dose of his anti-tropical rattlesnake serum, demonstrating that
antivenom could sometimes be used effectively for treating envenomation from
different species.
Using
crude venom to inoculate animals (often horses) will produce effective
antiserum, but it can be hard on the animals. In 1924, Gaston Ramon detoxified venom
by combining it with an aldehyde, such as formalin. Detoxified venom or raw
venom used for immunization could be combined with another chemical such as
aluminum hydroxide or sodium alginate to act as an adjuvant. Adjuvants slow the
release of venom and stimulate the immune response. The number of injections
needed to hyperimmunize an animal varies from 10 to 50 injections over a period
of 3 to 15 months. Blood samples are tested for the antibodies and, once an
acceptable level is reached, the animal’s blood can be collected, mixed with an
anticoagulant (often sodium citrate), purified, and prepared for distribution
as a liquid or a freeze-dried product [Figure 6–3]. The antivenom is usually said
to have a shelf-life of two years in the liquid form or 5 years in the
freeze-dried form. Dried antivenom, however, has a shelf-life of 15-20 years
and can remain effective much longer.
However, in a business move, and in order to move stocks of antivenin,
one company began shortening the shelf life to 5 years to encourage cash
flow. Many others followed suit. Antivenom is the only effective treatment for
snake envenomation. Unfortunately, its capacity to induce severe allergic
reactions in some patients concerned physicians.
INSERT
FIGURE 6-3.
Figure 6–3. Antivenom products for
snakebite. Photo by Ian Simpson.
Patients
receiving the antibodies may suffer from several types of reactions that
include an anaphylactoid reaction that is rapid and systemic and involves
swelling in the face and throat that can result in death. Such reactions need
to be treated quickly with epinephrine. Other reactions to antivenom are less
dangerous. Pyrogenic reactions induce a fever and need to be treated with
pyretics. Serum sickness may also occur and may be delayed up to two weeks
after exposure to the antibodies. Serum sickness is characterized by rashes,
swollen lymph nodes, hypotension, and other symptoms associated with allergic
reactions. These responses are often treated with corticosteroids and
antihistamines. Reactions to antivenom were reported to exceed 20% in patients
and this resulted in physicians delaying treatment and administering a dose of
antivenom that was too low to be effective.
Despite
this, a study done by Steve Offerman and colleagues in 2001 found the use of
polyvalent Crotalid antivenom was safe and should be used in treating patients
with moderate to severe envenomation from rattlesnakes. They used hospital
records from 65 patients who had received antivenom between 1988 and 1998. Allergen related side effects in those
receiving the antivenom were seen in 12 patients (18%) and in 11 of these the
reaction was limited to a rash. Only one patient (2%) required epinephrine.
It was discovered that by digesting the IgG
with an enzyme like pepsin or papain that the part of the antibody that
neutralizes venom can be separated from the rest of the molecule. This has
become known as fragment antibody binding or Fab. This process presumably
reduces the probability of adverse reactions to the antivenom. In October of
2000, the United States Food and Drug Administration approved a Fab antivenom
product as treatment for mild to moderate crotalid snake envenomation after
trials had been conducted from 1993 to 1996. CroFabTM was manufactured by
Protherics in Nashville, TN. Protherics began
using sheep instead of horses for antibody production. However, it has not yet
been demonstrated that humans have a lowered reaction to ovine antibodies or
antivenom produced by the Fab process. FabAV (fragmented antibody binding
antivenom) is a second generation antivenom. Unfortunately, CroFabTM currently costs US$1200 per vial, making it a
financially irresponsible alternative when one considers that anaphylactoid
reactions can be treated with a US$1 injection of epinephrine. This situation
is complicated by the facts that anaphylactoid reactions can occur very
rapidly, and CroFab has yet to be show to produce fewer unwanted side effects.
Purification
of crude serum by removing cellular particles and unnecessary proteins is done
with a centrifuge and precipitation of the antibodies is achieved with ammonium
sulphate or caprylic acid. The number of antibodies collected is twice as great
using caprylic acid and makes production more efficient and less costly. Currently,
India produces one million vials of antivenom using ammonium sulphate
precipitation. By changing to caprylic acid methodology, antivenom
manufacturers could double their output.
A
BBC report on August 31, 2000 reported a global shortage of antivenom due to
manufactures closing down their antivenom operations for economic reasons.
However, the loss of production was due to ‘snakebite experts’ close to the
manufacturers who called for more quality control with no real evidence that it
was needed. The manufacturers were using inefficient methods of production and
would not acknowledge the more efficient methods of production using caprylic
acid.
During
the first decade of the 21st century, the availability of antivenom in the USA
and other countries has been in short supply. In 2000 Federal inspectors found
"quality control" problems at the Wyeth Pharmaceutical plant in
Pennsylvania. Wyeth was the only producer of whole IgG rattlesnake antivenom
for US species. Production was halted until 2001, and the manufacturer was
forced to ration its remaining inventory, leaving some hospitals with very
limited supplies. In 2000, a Washington Post story cited a survey of Arizona
hospitals that had only 1,000 vials of antivenom on the shelves, when they
usually require twice that number. The litigious nature of medicine in the USA
has placed pressure on physicians to administer antivenom for any symptoms of
envenomation, including swelling and necrosis which are not controlled by
antivenom. This has resulted in the need for more antivenom on hospital shelves
even though it may not be necessary.
The
halt in production of the polyvalent pitviper antivenom was soon followed by
Wyeth’s announcement that it would cease production of antivenom in 2001. Note
that the Offerman study cited above showed that using polyvalent Crotalidae
antivenin was safe, but Wyeth had stopped production.
By
2002 it was apparent there was a shortage of antivenom in the USA. A University
of California Davis Medical Center press release that said that both horse and
sheep derived antivenom for rattlesnake bites were in short supply. Protherics
reported a problem with the product being “out of specification” as the result
of a short-term problem with the production process. But, by 2004 CroFabTM was
again readily available in the USA.
By
2009 there was no available whole IgG antivenom available in the USA. A study
by Eric Lavonas and colleagues at the Rocky Mountain Poison and Drug Center
examined the medical records of patients who had been given FabAV between 1996
and 2008 in an attempt to determine its effectiveness for patients with severe
envenomation. Their conclusion was FabAV therapy was well tolerated and is
appropriate for managing severe envenomations.
The
six Indian manufacturers of snake antivenom combined produce more than 1
million vials of polyvalent venom per year. The average treatment per snakebite
envenomation is 15 vials of antivenom. There are about 80,000 envenomations in
India and therefore a need for 1.2 million vials. Indian manufacturers
currently produce enough antivenom so there is probably no shortage in that
country. A trial of effective protocols in West Bengal reduced the use of
antivenom by 20,000 vials per year at one District hospital. Ian Simpson and Rob ert
Norris reviewed the instructions accompanying the antivenom and found that
reliance on those instructions would waste antivenom. But of greater concern,
following the instructions would actually cause more harm to the victim. The
instructions included recommendations for using rubber ligatures, making deep
incisions at the bite site, and applying suction by mouth or mechanical device.
Furthermore, the instructions suggested the use of magnesium sulfate to
“eliminate tissue fluid containing the venom” and they advocated strychnine for
the treatment of shock. All of these treatments have been applied in the past;
they often are described in the older snakebite literature, and they have not
been considered effective or safe since the early to mid-20th century. Simpson
and Norris also found problems with the brochures’ lists of anticipated
symptoms and the instructions for dosing and the timing of dosing. They made
recommendations at the Indian National Snakebite Protocol Consultation Meeting
in 2007 with the hope that all manufacturers would adopt their suggestions for
modernizing their instructions. Both Indian and Pakistan now have a national
treatment protocol.
Bites
from the Martinique Fer-de-lance (Bothrops lanceolatus) between 1993 and 2001
were treated effectively with antivenom, but three of 10 patients treated with
the antivenom between 2003 and 2004 developed cerebral infarctions. When the
antivenom was tested on mice it was found to be less effective than specified
by the manufacturer. Some of the antivenom was more than 15 years old. In 2007
the Health and Social Development Administration on the Caribbean island of
Martinique was making special requests for people to collect the Fer-de-lance so
that they could replenish antivenom stocks.
An
Australian study found antivenom to be ineffective in controlling coagulopathy
(excessive bleeding) from elapid bites and reported the administration of fresh
frozen plasma was needed to restore coagulation factors in the blood, which
takes the liver about six hours. A study of expired antivenoms looked at the
activity of expired taipan, brown snake, and polyvalent antivenoms. While all
of the antivenom batches remained partially active they showed some
deterioration in activity and binding over time. All tested taipan antivenom,
including one 15 years expired, still prevented blood clotting. Brown snake
antivenoms also prevented clotting, except for two vials that were 10 years
old. Thus, antivenom remains effective
long past the expiration date.
The
WHO snakebite study discussed above clearly considers snakebite a neglected
issue, They point out that antivenom for snakebites is not widely available in
many countries, and that its availability is not sustainable. Simpson and Norris
took exception and note that the lack of physician training, poor advice from
experts, and a lack of economic analysis are part of the problem. In Africa one
antivenom producer made a product called ‘Bitis’ for viper bites from the Puff
Adder (Bitis arietans) and the Rhinoceros Viper (B. nasicornis). Another
product called ‘Naja’ provided treatment for envenomation by the Black-necked Cobra
(Naja melanoleuca) and the Mozambique Spitting Cobra (Naja mossambica). Both
antivenoms are recommended for use in Mozambique. However, Puff Adder and Mozambique
Spitting Cobra envenomation produce similar symptoms (swelling) and doctors are
often unsure as to which antivenom to use. An Indian manufacturer of antivenom
wanted to market its product in Africa so it obtained the product insert of an
African antivenom producer and copied its species list, selling Indian
antivenom in Africa. Yet a third supplier who attended the WHO meeting supplied
ineffective antivenom to Africa, and another entrepreneur provided outdated
advice on how the product was to be used. The concept of species specific
proteins may be missing here. Simpson and Norris pointed out that the global snakebite
problem has not been neglected so much as misunderstood. Newer techniques for
antivenom production as well as physician training are critical to improving
the treatment for snakebite.
Considering
that the fundamentals of antivenom production have been known for a century,
the current problems seem unnecessary and unconscionable. Simpson and Norris
have laid out a marketing mix that can make antivenom both sustainable and
available and would allow manufacturers to produce a vial of IgG antivenom for
a reasonable cost (US$8 to $42 per vial) depending upon volume. So, why is
reasonably priced whole IgG antivenom not available in the USA? This is a
question that needs investigation, considering the fact that Fab produced
antivenom has not been demonstrated to have reduced side effects or be more
effective at reducing the symptoms of envenomation.

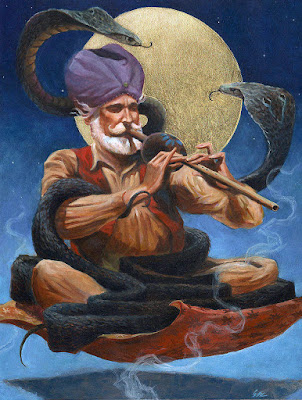
Comments
Post a Comment